Interoperability reference architecture
HL7 v2, HL7 v3, and HL7 FHIR are three of the most common healthcare messaging standards used today. This section highlights architectures for each.
HL7 v2
In practice, HL7 v2 tends to have reasonable structural standardization, but weak semantic interoperability. Structurally, HL7 v2 messages consist of one or more segments delineated as separate lines. Within each segment, fields are pipe-delimited. Semantically, the contents of HL7 v2 messages may use any number of standard vocabularies or lack externally linkable terms or codes entirely. If using HL7 v2, consider automated ways to map to standard ontologies, such as using NLP algorithms trained on medical text.
The Minimum Lower Layer Protocol (MLLP) is a common transport standard used for HL7 v2 interoperability. MLLP streams bytes using TCP/IP and uses special header and trailer (such as a footer) wrappers to signify the beginnings and ends of messages. Notably, the MLLP does not natively provide encryption. However, in recent years, many interfaces have started supporting MLLP over TLS for added security. For interfaces that do not support TLS, additional measures must be taken to verify encryption of data in transit.
An HL7 v2 interoperability architecture may leverage the HL7 v2 APIs of a source system, like an EHR. To provide end-to-end encryption between the source system and target system, it’s a best practice to use a VPN tunnel or secure protocols like SSH File Transfer Protocol (SFTP), as MLLP may not provide TLS. The source system may asynchronously send batches of messages to an encrypted Amazon S3 bucket, or may synchronously exchange messages with a target integration service, as shown in the following figure.
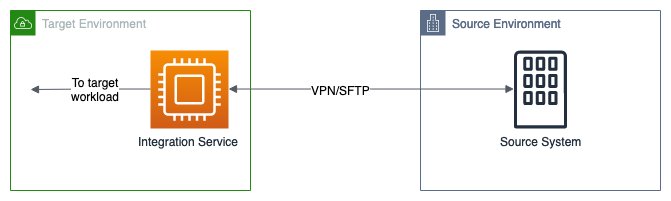
A common HL7v2 interoperability architecture where the integration may exchange HL7 v2 messages through a VPN tunnel or SFTP. MLLP over TLS can help keep messages encrypted in transit.
HL7 v3
The HL7 v3 standard is commonly used for exchanging Continuity
of Care Document (CCD) and Consolidated Clinical Document
Architecture (C-CDA) messages. These messages are often
exchanged using Cross-Enterprise Document Sharing (XDS)
transactions, which are based on web services. Amazon API Gateway can be used to create a web service to support these
XDS transactions such as ITI-41. TLS with
certificated-based
authentication
FHIR
The following diagram illustrates a representative FHIR interoperability architecture, which presents an integration point in front of one or more systems of record, typically within a provider or payer organization.
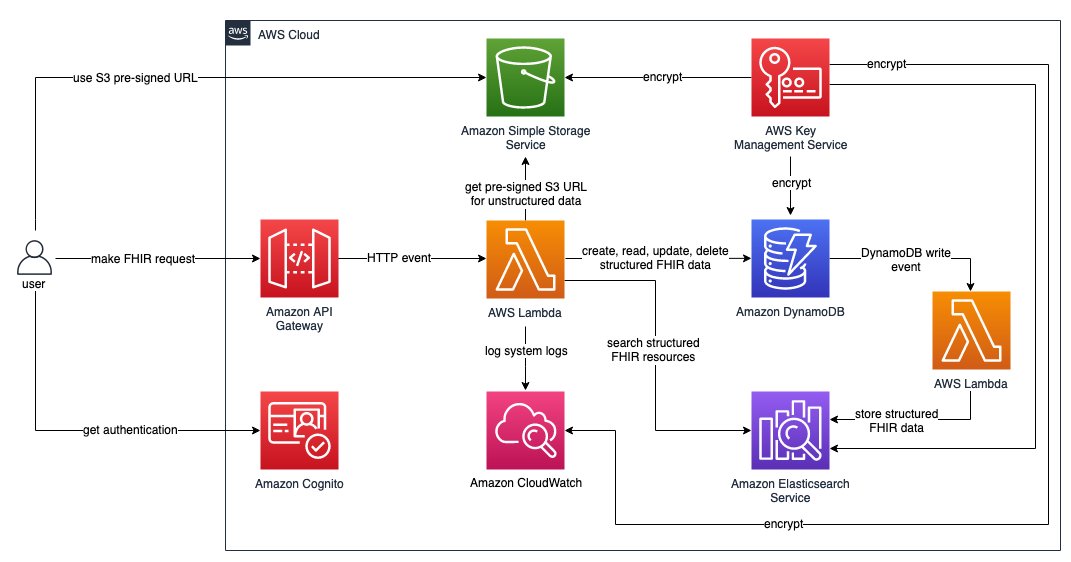
Example FHIR enabled interoperability architecture.
-
An API or server endpoint is made available for integration with other systems or users. A managed API service, like Amazon API Gateway, ensures scalability and high availability. Restrict network access to the API if possible and use a web application firewall to filter malicious requests.
-
Inbound requests are authenticated with OAuth
or a service like Amazon Cognito to verify that sensitive health data is only exchanged with appropriate parties. -
Inbound payloads are checked for conformance to relevant structural interoperability standards, ensuring the safety and integrity of data exchange.
-
Data may be written to or pulled from systems of record within the organization hosting the interoperability architecture.
-
Many systems of record host health data in proprietary formats and schemas. Therefore, interoperability architectures perform some transformations to map data elements to and from the interoperability standard.
-
The architecture may store the exchanged health data using a database service like DynamoDB, or it may exchange data without persisting it.
-
AWS HealthLake
enables use cases that require enrichment of health data in FHIR format or downstream analytics and machine learning. AWS HealthLake can improve semantic interoperability by applying natural language processing (NLP) to link concepts in unstructured data to terms in standard health ontologies, like ICD-10-CM, SNOMED CT, and RxNorm.